Clinical Examination of the Painful Hemiplegic Shoulder
Although the examination procedures and techniques generally remain uniform when assessing both neurological and orthopedic clients, depending on the severity of hemiparesis, modifications to certain tests may be required. For example, if the neurological client’s upper limb is severely impaired (Brunnstrom Stage 3 or lower), it is not impossible, but certainly more challenging to identify the lesion site when using standard clinical examination techniques. Synergistic influences will impede the client from performing key soft tissue tests such as active and resistive movements effectively. The client’s inability to isolate joint movement may result in misleading outcomes secondary to the spastic nature of the limb (i.e., cocontractions, lack of motor control). With respect to a flaccid or severely weak client, extreme loss of movement can hinder the ability to provoke his or her symptoms during active motion tests. Therefore, the clinician must consider alternative strategies and testing modifications to identify the pain source. Palpation techniques can become even more useful with this population when adaptations are necessary.
In my humble opinion, clinicians who are seeking post-graduate training in the field of diagnosis and non-operative treatment of soft tissue lesions should look no further than Dr. James Cyriax. Cyriax, commonly referred to as the father of orthopedic medicine, was an Internist and Orthopaedic Surgeon in England in the early 20th century. As a young physician, he observed that his superiors could not explain how they arrived at a musculoskeletal diagnosis nor specify what the problems were. Therefore, he proceeded to develop a series of simple objective clinical exams that would effectively diagnose soft tissue musculoskeletal lesions. Dr. Cyriax’s teachings are still widely popular today and can be beneficial when treating clients with pain and hypomobility.
Inert Structures
Cyriax once said “a healthy structure functions painlessly; a faulty structure does not. He discussed how the main emphasis of the examination is to find the movement that provokes the pain that the client is experiencing. This is possible when one understands the distinction between inert and non-inert (contractile) structures. For instance, inert structures lack the ability to contract and relax. These structures are the joint capsule, ligaments, fasciae, bursae, dura mater, and dural sheaths. Inert tissue can only be provoked while put under tension by stretching. When a patient relaxes her affected limb (contractile structures are unloaded) and the clinician performs the passive movement for the client, the inert structures are stretched. If the passive motion is painful, then the inert structures are at fault.
End-Feel
Every joint has a characteristic end-feel for each motion depending on the structures restricting that motion. When assessing the joint passively at end-range, the clinician must rely on the specific sensations in his or her hands known as the end-feel. The quality of the resistance that the clinician feels at end range is determined by the structure restricting the movement, lesion, gender, age, general flexibility, and how the examiner performs the test.
There are 3 different qualities of end-feel: soft, firm and hard. If a clinician is unable to test the end-feel due to pain then it is categorized as an empty end-feel. An example of soft end-feel would be soft tissue between long bones (i.e., elbow flexion). A firm end-feel example would involve a joint movement similar to shoulder external rotation or hip abduction since it has more of a ligamentous feel. Finally, an example of hard end-feel would involve a motion with a bony “stop” like elbow extension or knee extension.
Various types of end-feels correlate with various disorders. A clinician can differentiate between a normal end-feel and a pathological end-feel. For example, if the end-feel for elbow extension is not considered hard, then the joint would not be considered normal. Therefore, the clinician must have a good working knowledge regarding pathological end-feels since the quality of the resistance felt is an important diagnostic indicator.
Non-inert Structures
In addition to inert structures, another key area to assess will be non-inert (contractile) tissue. When a client exerts his or her muscles to maximum voluntary contraction, no tension falls on the inert structures. Instead, the strain is located on the muscle or muscle group responsible for the particular movement. Pain that occurs during muscle contraction is more likely to indicate a lesion in the muscle belly. Pain that occurs upon release of a contraction is more likely to indicate a lesion within the tendon.
Physical Examination and Interpretation
The main examination principles outlined below are based on the principles of Cyriax and more recently, the International Academy of Orthopedic Medicine (IAOM). The examination is specifically performed to identify the source of pain reported by the neurological client. This examination will not replace your comprehensive neurological evaluation, but will be used as an adjunct to specifically identify the lesion source at the shoulder.
The clinical examination consists of the initial impression, history, active movements, passive movements, resisted test, palpation, and special tests.
A. Initial Impression
Appropriate exposure of both upper extremities will be necessary for adequate inspection of the shoulder. Typically, a clinician will look for attitude, deformities, swelling, discoloration, and muscle characteristics. Painful shoulders are usually positioned higher or in a protracted position as compared to the opposite side. Atrophy noted in the supraspinatus or infraspinatus region (excessive prominence of the scapular spine) can indicate a complete tear, nerve lesion or weakness from the hemiparesis. Atrophy noted over the deltoid is typically related to axillary nerve involvement or paresis (possible subluxation). Scapular asymmetry may indicate weakness of the scapular stabilizers. Enlargements of the SCJ and ACJ can be due to hyperostosis and should be noted. Finally, discoloration from bruising may indicate recent fracture or cuff injury. Although the above is not an exhaustive list and only used as examples, your initial impressions should suggest which part of the examination should receive additional scrutiny.
B. History
In addition to conducting the physical examination, an accurate diagnosis can be established by a obtaining a clear and chronological history. In general, a client’s chief complaint and age often suggests the correct diagnosis. For example, a 70-year old (non-neurological) with rotator cuff weakness and shoulder pain probably has a rotator cuff tear. A 20-year old college pitcher complaining that her shoulder feels like it is “coming out” probably has instability. A 50 – year old high level stroke survivor complaining of pain during elevation may have rotator cuff tendinopathy secondary to external impingement. It will be essential to identify the patient’s age, occupation, onset, location and intensity of pain. Knowing if the pain originated following a traumatic event, where the pain was first felt, where it has spread since, and the general progression of the disorder will also be important.
C. Cervical Screen
A quick screen will rule out cervical involvement. The key question that the clinician must answer is - do the cervical movements provoke the symptoms that the patient is experiencing? Radiculopathy caused by irritation or compression of the C5 nerve root often results in referred pain over C5 dermatome. In addition, C5 and C6 spinal nerves innervate most of the GHJ (lateral-proximal aspect of shoulder is a very common pain location).
Active, passive, and resisted tests will rule out the neck from any involvement. Motions to assess include flexion, extension, right rotation, left rotation, right lateral flexion, and left lateral flexion.
D. Shoulder Girdle (screens ACJ, SCJ, STJ)
Similar to the cervical screen, the clinician should test the shoulder girdle for pain provocation. The shoulder girdle comprises of the acromioclavicular joint, sternoclavicular joint, and scapulothoracic junction. The client should actively perform the following movements.
- Shrug shoulders (elevation)
- Depress girdle
- Protract
- Retract
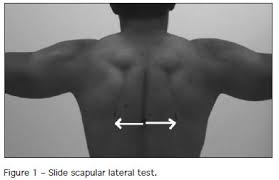
To evaluate any muscular imbalances and/or areas of focal atrophy that possibly can be linked to the underlying pain, the client should also perform Kibler’s Static and Dynamic Scapulothoracic Junction Tests.
Static Tests
Evaluation of the client occurs in the standing position with both arms resting comfortably at the side of the body. The clinician should note the outline of the scapula and compare both sides for any asymmetries. After examination of the client with the arms in adduction at the sides of the body, the next static position is with the client’s hands on his hips. If the client is unable to actively position the affected hand on the hip due to weakness, then the clinician should assist manually. This position creates slight internal rotation and abduction of the glenohumeral joint. It also relaxes the arms and allows the clinician to observe any asymmetry or atrophy along the scapular border.
Dynamic Test
After the static tests are completed, the client is asked to elevate both arms in a self-selected plane of movement. The clinician is observing the scapula during concentric elevation and eccentric lowering. Clients with scapular dyskinesis will most likely experience superior movement of the scapula (shoulder shrug) during concentric elevation and/or prominence of the inferior angle and medial border during the eccentric lowering phase.
Asymmetry indicates muscular imbalance to the scapular stabilizers (rhomboids, trapezius, serratus anterior). Often times, the asymmetry is identified during the setting phase (0-60 degrees).
Note: the Scapulothoracic Dynamic Test is most meaningful for neurological clients that can demonstrate active arm elevation (3 or 3-/5 muscle strength). Without the ability to actively raise the arm sufficiently, the clinician will be unable to examine the scapular movements and associated muscle group contributions.
E. Active Arm Elevation
When assessing arm elevation, the clinician is looking specifically for weakness and pain. Although active tests will be appropriate for clients suffering from mild to moderate hemiparesis, it may not be effective for individuals with severe hemiparesis due to their decreased motor control.
Active Unilateral and Bilateral Movement - For arm elevation, the client should elevate (flex or abduct) the arm naturally so the clinician can observe the client’s movement preference. Feel free to repeat the test in the other plane so both motions are assessed. Finally, have the client actively raise both arms simultaneously. Unilateral elevation should be greater than bilateral due to upper thoracic rotation.
Painful Arc Test – with the arm positioned in 0°of abduction, the client elevates the arm slowly. During elevation, if the client experiences pain, followed by no pain as the elevation continues, then a painful arc sign is noted. Subacromial painful arc usually occurs between 60-120 degrees of elevation. Typically, one or more of the subacromial structures between the head of the humerus and the roof of the shoulder are impinged.

Structures at risk:
- Supraspinatus insertion (superior or lateral part)
- Infraspinatus insertion (superior or lateral part)
- Subscapularis insertion (proximal part)
- Long head of biceps tendon or sheath
- Subacromial Bursa
Questions to Consider When Assessing Active Movement Include:
- Does a hypomobility exist?
- Any pain noted during active elevation? If so, where in the ROM?
- Does the client exhibit a painful arc?
Note: Client’s with reported pain at the C5 dermatome during active elevation are most commonly suffering from a subacromial lesion. Further testing will be needed (passive, resisted, and special tests) to confirm the exact lesion site.
F. Passive Tests
Many neurological clients exhibit increased spasticity and soft tissue shortening with their humeral adductors and internal rotators. These movement restrictions often result in adaptive changes to the capsule and glenohumeral joint ligaments causing increased shoulder pain and limited external rotation. When assessing passive motion, the clinician is looking at available motion and provocation of pain. The amount of motion found during the passive evaluation is compared with the active motion. If a hypomobility exists during passive tests, differentiation is made between capsular and noncapsular patterns as well as end-feel.
As discussed in the previous article, capsular pattern is synonymous with frozen shoulder or adhesive capsulitis. It consists of greater limitation of external rotation than abduction and a greater limitation of abduction than internal rotation, in a ratio of 3:2:1, respectively. Hemiparetic clients with severe limitations of movement often develop a capsular pattern due to progressive adaptive shortening of the collagen. Conversely, many mildly impaired neurological clients complaining of shoulder pain typically present with a non-capsular pattern (limitation of movement that does not correspond to the fixed proportional limitation of the capsular pattern). In other words, the entire joint capsule is not affected and a client may only have restrictions with one part of the capsule (i.e., unable to place hand behind back to grab wallet due to a tight posterior capsule).
Passive Arm Elevation Test - The clinician will passively elevate the client’s arm while stabilizing the contralateral shoulder girdle. At the end of the range, the clinician will provide slight over pressure. This test specifically is looking for hypomobility or pain at the acromioclavicular or sternoclavicular joint.
Passive Arm Elevation (with overpressure) - the clinician will passively elevate the client’s arm and provide posterior and medial overpressure while fixating the ipsilateral scapula. Pain noted with posterior over pressure may be due to subacromial bursitis or a lesion of long head of biceps. Whereas pain noted with medial over pressure may be due to internal impingement (infra/supra tendon impinging on labrum).
Note: the above end-range tests may not be possible for client’s suffering from severe hemiparesis due to spasticity and soft tissue shortening. Therefore, additional tests may be required.
Passive Glenohumeral Abduction - To evaluate available humeral range of motion and capsular elasticity, the clinician can perform passive abduction by stabilizing the lower angle of the scapula with his or her thumb and passively elevating the involved arm (with elbow bent) until the scapula is felt to rotate. Due to the provocative nature of this test, the clinician will not provide overpressure at end range as the humeral head will have made contact with the acromion possibly causing further pressure and additional pain.
Passive External/Internal Rotation - Two final passive movements for the joint are external and internal rotation. For passive external rotation, the clinician stands obliquely behind the patient, next to the side being tested. The clinician flexes the patients elbow to 90°,and stabilizes it next to the body, while the arm remains in 0° of abduction. With the ipsilateral hand, the clinician grasps the patient’s forearm and passively rotates the shoulder externally. The clinician’s contralateral hand is placed on the patients opposite shoulder to stabilize the body and avoid any axial rotation. Slight overpressure is exerted at the end of the motion. Pain during passive external rotation may result from an infraspinatus rupture. If passive external rotation is not limited, but only painful, the cause most likely will be due to stretch on anterior structures (capsule/subscapularis insertion) and/or acute bursitis. Pain may also be due to muscle shortening (trigger points) of the adductors and internal rotators from spasticity and disuse.
With respect to passive internal rotation, the clinician will stand behind the patient, opposite the side being tested. The affected humerus is prepositioned in submaximal extension and adduction (hand behind back). The clinician stabilizes the patient’s elbow against his or her body. Without extending the patient’s arm, the clinician performs internal rotation exerting slight overpressure at end range. When affected-side scapula begins to move, the client has reached the end range of the joint. Pain during passive internal rotation can result from ACJ pathology. Additionally, pain may be caused from stretching the affected infraspinatus/supraspinatus or posterior capsular shortening.
G. Resisted Movements
Depending on the level of neurological involvement, resistive tests may prove challenging if one is unable to adequately recruit and isolate individual muscles. A client suffering from moderate to severe spasticity may demonstrate co-contractions during isometric resistive tests, which will most likely lead to dubious results. For example, let’s assume we are evaluating a severely impaired hemiplegic client that exhibits a flexor synergy pattern and reports C5 dermatome pain. As the client attempts to elevate his arm, his movement depicts the stereotypical pattern of shoulder abduction in combination with elbow flexion. To rule out the supraspinatus as a possible source of pain, the clinician normally would isolate the muscle by testing resistive abduction with the arm at neutral (side of body). However, in this example, resistive abduction cannot be isolated due to abnormal tonal influences. If the client reports pain at the shoulder during resistive abduction, the clinician will be unable to confirm if the supraspinatus is at fault or possibly long head of biceps since both muscles are firing simultaneously due to the synergistic coupling. Therefore, to avoid ambiguity or false-positive findings, a clinician must perform additional tests to further investigate the source of pain.
When testing contractile structures, the client will perform a series of isometric resisted movements to the targeted muscles in an effort to reproduce the symptoms. To keep the inert structures free from stretch, no movement should take place at the joint during the isometric tests. In addition, the client must provide maximum voluntary contractions during the tests to increase the possibility of irritation and strain. There are 5 resisted movements that can confirm if contractile structures are responsible for the client’s pain.
Adduction – client’s arm is positioned in 0°of abduction (arm at side of body). The clinician attempts to resist adduction by pulling the arm (above the elbow) away from the body while the client resists. Muscles tested include the pectoralis major, latissimus dorsi, teres major and teres minor. When tested positive for pain, teres major and minor are rarely involved.
Abduction – client’s arm is positioned in 0°of abduction. The clinician attempts to resist abduction by pushing the upper arm in towards the side of the body while the client resists. The movement is resisted above the client’s elbow while counter-pressure is applied to the opposite trunk. Muscles tested include supraspinatus and deltoid. When tested positive for pain, the deltoid is rarely affected.
External Rotation – client’s arm is positioned in 0°of abduction with elbow flexed at 90°. The clinician attempts to resist external rotation by pushing the forearm in towards the abdomen while the client resists. Muscles tested are infraspinatus, supraspinatus, and teres minor. When tested positive for pain, supraspinatus is less often involved and infraspinatus is usually the culprit. Occasionally, both resisted external rotation and resisted adduction are positive for pain showing teres minor to be at fault.
Internal Rotation – client’s arm is positioned exactly like the resisted external rotation test. The clinician attempts to resist internal rotation by pulling the forearm away from the abdomen while the client resists. Muscles tested are subscapularis, pectoralis major, latissimus dorsi, and teres major. When tested positive for pain, subscapularis is most commonly involved followed by pectoralis major and latissimus dorsi.
Elbow Flexion – client’s arm is positioned similarly to external and internal rotation (0° of abduction with elbow bent). The clinician attempts to resist elbow flexion by pushing the forearm down toward the floor. The bicep muscle is tested in this position. Resisted supination of the hand can be combined with elbow flexion to stress the muscle even further. When tested positive for pain, the long head of biceps is usually affected. However, the short head is also activated and migrates proximally which could compress an inflamed bursa resulting in pain.
Elbow Extension – client’s arm is positioned similarly to elbow flexion. The clinician attempts to resist elbow extension by pushing the forearm up toward the upper arm. The triceps muscle is tested in this position, which is rarely at fault. Pain from this movement is usually in the C5 dermatome and thus not localized at the triceps. During resisted elbow extension, the triceps pulls the humerus upward causing the already inflamed subacromial tissues to become compressed.
H. Palpation
Although palpation is a widely used technique by clinicians to determine the presence and location of pain, results can be misleading since most pain symptoms are often referred on a segmental basis. Cyriax once said “effective treatment must be delivered not just to the right tissue, but the right part of the right tissue: the lesion itself”.
Keeping this in mind, based on the results of the examination, the suspected affected structure should be localized and palpated for warmth, swelling, tenderness and pain. Even though palpation results are not fool proof, it may help rule in, or out, specific lesion sites in question.
I. Common Special Tests for Hemiparetic Shoulder Pain
Once the basic functional examination is complete, additional special tests may be required to confirm a diagnosis. Although there are numerous special tests available for the shoulder, this article will discuss a few that are most relevant for neurological clients.
Pull Tests for Bursitis – if the client demonstrates a positive resistive test (abduction, IR, ER) the clinician should perform the Pull Test to differentiate between a tendinopathy or bursitis. The clinician should repeat the painful resisted tests while the clinician displaces or inferiorly pulls on the humerus (i.e., traction). If the resisted test is no longer painful with the inferior displacement, but painful without the pull, then the bursa is affected.
Hawkins-Kennedy Impingement Test -This test creates mechanical compression of the rotator cuff tendons against the coracoacromial arch and the coracoid process. The clinician places one hand on top of the shoulder being tested to stabilize the girdle while elevating the humerus to 90° in the plane of the scapula. The clinician then passively internally rotates the humerus to end range of motion or until reports of pain. The test is positive if pain is reported in the superior-lateral aspect of the shoulder.
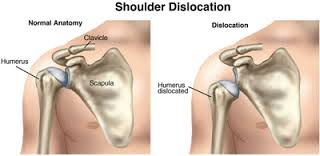
Laxity Tests - Since many hemiparetic clients experience weakness following a neurological injury, it is not uncommon to observe hypermobility or instability at the glenohumeral joint. Paralysis of the shoulder girdle will comprise the dynamic stability of the rotator cuff muscles leading to an unstable joint.
3 Main Directions of Instability
- Anterior Instability: humeral head migrates excessively in an anterior direction relative to the glenoid.
- Inferior Instability: excessive inferior movement of the humeral head relative to the glenoid.
- Posterior Instability: excessive movement of the humeral head in a posterior direction relative to the glenoid.
Note: The most common type of instability associated with hemiplegia is in an inferior direction (subluxation). An Inferior subluxation occurs when muscle weakness leads to a downward rotation of the scapula in relation to the thorax. The labrum and inferior portion of the glenoid fossa can no longer provide sufficient support to secure the humeral head into the glenoid. In addition to the faulty mechanics at the scapula, the proximal migrators of the shoulder (deltoids) are no longer able to support the weight of the arm. Gravitational forces applied to the weakened arm stretches the inert and non-inert structures to the point that the humeral head migrates distally below the glenoid fossa.
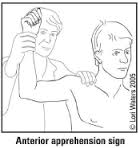
Apprehension Test – The clinician passively elevates the affected arm into 90° abduction and full external rotation, while slightly horizontally abducting/extending the arm just posterior to the coronal plane of the client’s body. If the client can tolerate this position, then pressure is applied to the posterior aspect of the client’s shoulder, pushing the humeral head in an anterior direction to further provoke the client’s extremity. A positive test indicates anterior glenohumeral instability.
MDI Sulcus Sign – With the client’s arm at the side of the body, the clinician grabs the distal aspect of the humerus with one hand while placing the thumb and index finger on the anterior and posterior lateral corners of the acromion with the other hand as a reference. The clinician then provides several quick, rapid pulls in a inferior direction while looking for production of sulcus.
In closing, with new scientific advances in neurorehabilitation technology, many clients suffering from UMN injuries are experiencing meaningful progress in motor recovery and Activities of Daily Living (ADL). Despite the optimistic outlook, an area that continues to be disconcerting is hemiparetic pain management. Generally, a clinician specializing in neurological rehabilitation does not typically have a strong background or understanding in orthopedic medicine. This can be quite problematic for a stroke client that is experiencing undiagnosed joint pathology resulting in pain and limitation of movement.
From initial impressions to special tests, a comprehensive examination is required to properly evaluate a painful shoulder. Hemiparetic shoulder pain continues to be challenging for clinicians and patients. There are numerous clinical conditions and pathologies (arthritis, rotator cuff tears, trigger points, spasticity) that can cause joint hypo/hypermobility and pain. In order to provide lesion specific treatment strategies, a thorough understanding of musculoskeletal system as well as joint specific diagnostic techniques must be appreciated.

Henry graduated from D’Youville College in Buffalo, NY in 1997 with a Masters degree in Occupational Therapy. He has worked in a variety of clinical settings including home health, acute, sub-acute, and outpatient rehab. Prior to leaving Burke Rehabilitation Hospital in New York in 2002, he worked as a clinical specialist in orthopedic medicine and manual therapy of the Upper Quadrant. After leaving Burke, Henry co-founded Saebo with the goal of creating innovative and life changing solutions for the physically impaired population. He currently holds over 15 patents with products that have helped over 30,000 clients regain function. Saebo’s name is an acronym for Henry’s grandmother “Sarah Eileen Booth”. Her entire life was dedicated to providing a hand to others in need. Saebo’s mission is to match her spirit, dedication, and desire to help others.
___________________________________________
Whether you are a caregiver, occupational therapist or even a stroke survivor yourself, Saebo provides stroke survivors young or old access to transformative and life changing products. We pride ourselves on providing affordable, easily accessible, and cutting-edge solutions to people suffering from impaired mobility and function. We have several products to help with the stroke recovery and rehabilitation process. From the SaeboFlex, which allows clients to incorporate their hand functionally in therapy or at home, to the SaeboMAS, an unweighting device used to assist the arm during daily living tasks and exercise training, we are commitment to helping create innovative products for stroke recovery. Check out all of our product offerings or let us help you find which product is right for you.
All content provided on this blog is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition. If you think you may have a medical emergency, call your doctor or 911 immediately. Reliance on any information provided by the Saebo website is solely at your own risk.



